RADIATING PAIN and/or NUMBNESS DOWN THE LEGS as a consequence of worn-out discs
‘Doctor, for years I have had pain in my lower back and I could live with it, yet now I also have pain going down my legs and that I cannot take anymore’
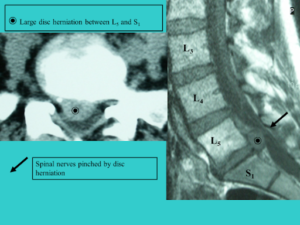
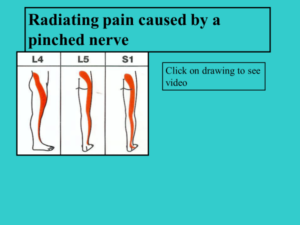
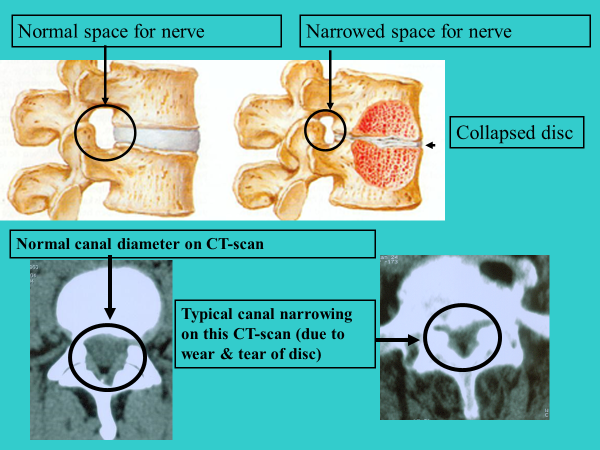
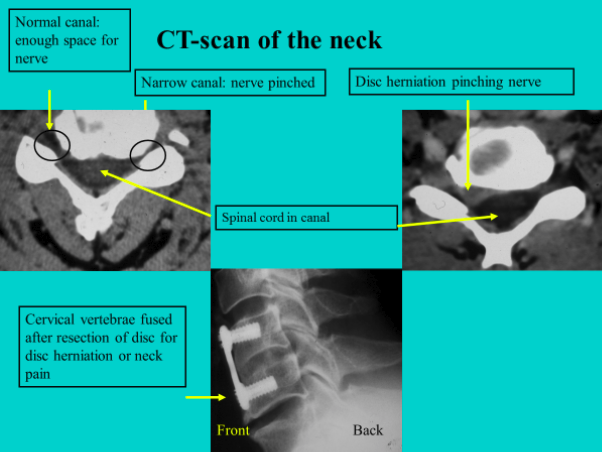
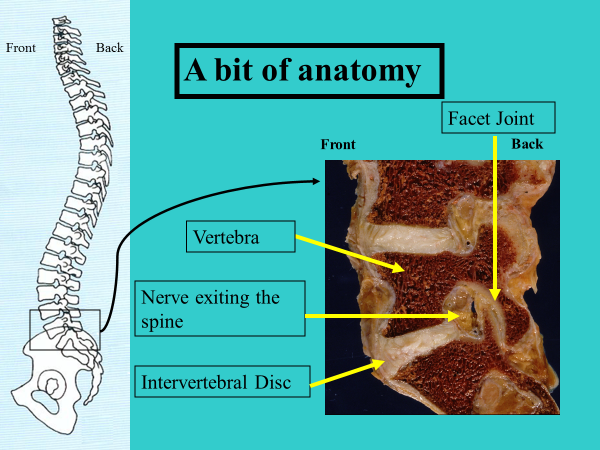
Due to wear and tear, the discs will decrease in height and bulge all around (just like a flat tire). As a consequence the disc will bulge (protrusion) and the vertebra above will come closer to the vertebra below. This causes a reduction in the size of the opening through which the nerves leave the spine. When such a nerve becomes truly squeezed, there will be a burning sensation with numbness or a feeling of pins and needles in that part of the leg for which this specific nerve is responsible. Each nerve goes indeed to a specific part of the leg, and by indicating where the changes are on the leg, the patient makes clear to the spine surgeon which nerve is involved. After some time, there can also be pain radiating down the leg as well as a typical diminution of the walking distance (neurogenic claudication).
In the beginning, the treatment is best followed by the general practitioner. Not only radiographs and scanners will be ordered, but also tests of the nerves such as EMG (insertion of tiny needles in the leg to analyse the function of the nerves). On the treatment menu you will find: medication, dieting, cease smoking, back muscle and abdominal muscle exercises, osteopathy, physiotherapy, acupuncture, epidural infections, a lumbar belt, improvement of work surroundings, a better bed etc
If all this does not help, one could wonder ‘CAN AN OPERATION BRING IMPROVEMENT?’
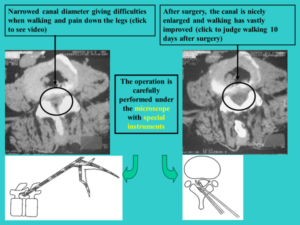
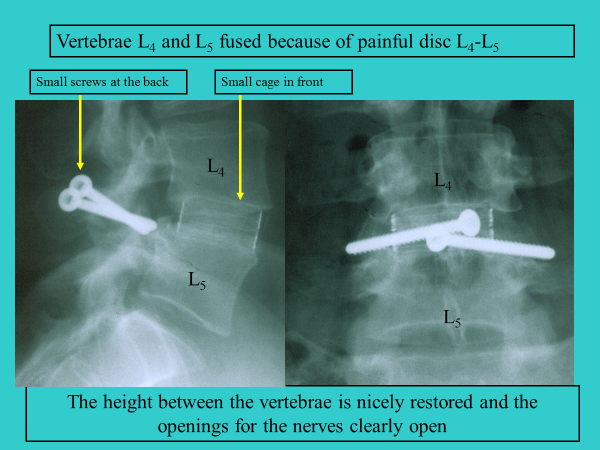
In most cases, yes. The principle consists of enlarging the opening through which the nerves pass on leaving the spine. This is being done WITHOUT altering the mechanics of the back. The discs and facet joint remain unharmed. The current state of the art techniques allow us to say that the odds that someone would feel significantly better at, let’s say some months after surgery, are around 95%. This does not mean that a specific person will be 95% improved, but that out of a hundred operated people, 95 are satisfied and 5 disappointed. These are mostly patients who either waited too long with their surgery, or those who form a large scar around the nerves (fibrosis) in the operated area. Strangely enough, these patients often also claim to have less back pain, whereas this was not the primary aim of the surgery.
The operations are performed under general anaesthesia, are not really painful, and the hospital stay is only a few days. Patients walk home from the hospital and active revalidation is seldom required. Elderly patients who have nobody waiting for them may benefit from a short stay in a revalidation centre, prior to going home.